AI-Native Prior Authorization for Rehab Therapy Clinics
Automate 80% of workflows, reduce denials by 75%, and secure approvals one week before appointments—all while preparing for CMS’s 2026 mandate.

Cut authorizations wait time from weeks to minutes

Automate PA submissions, reduce staff overload instantly

Slash claim denials with correct documentation upfront

Real-time PA status updates — no guesswork






80%
Prior Auth Requests Automated

75%
Fewer Denials Across Clinics
30+
Minutes Saved Per Auth Submission
95%+
Accuracy On Eligibility Matches
Trusted by leading rehab therapy clinics
















How SPRY’s Prior Authorization & Eligibility Works
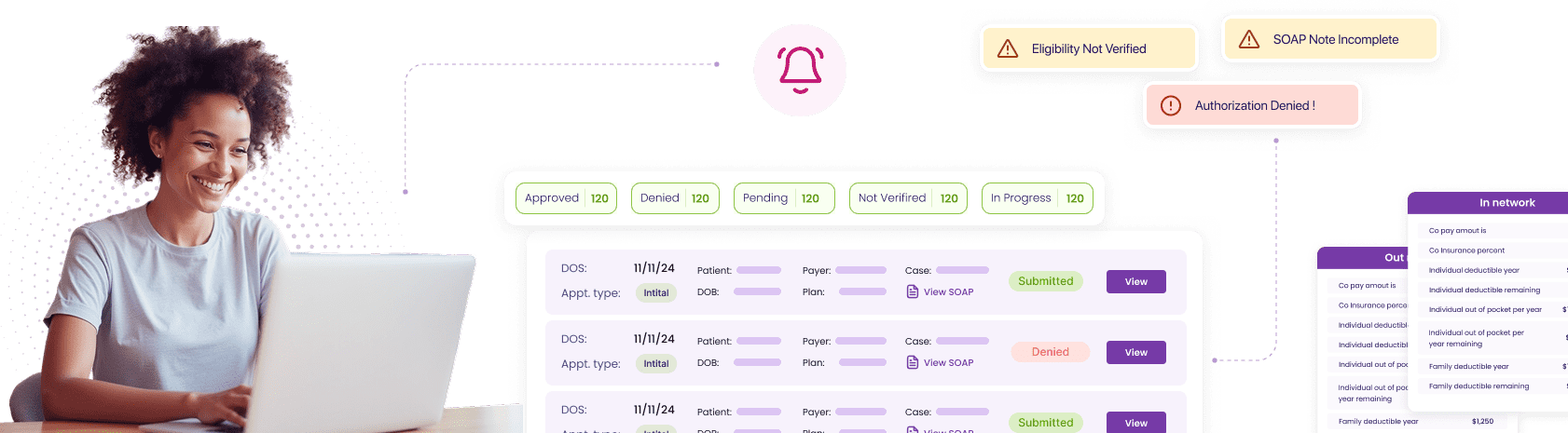
Centralize Every Insurance Workflow in One Dashboard
Streamline insurance operations by unifying eligibility, coverage, and authorizations in one system—eliminating portal-hopping and manual entry.
Accelerate Approvals and Prevent Costly Administrative Errors
Automate submissions with AI that files requests, attaches documentation, and flags issues early.

Deliver Real-Time Eligibility Results to Your Front Desk
Confirm coverage instantly with copays, deductibles, and limits verified at scheduling.
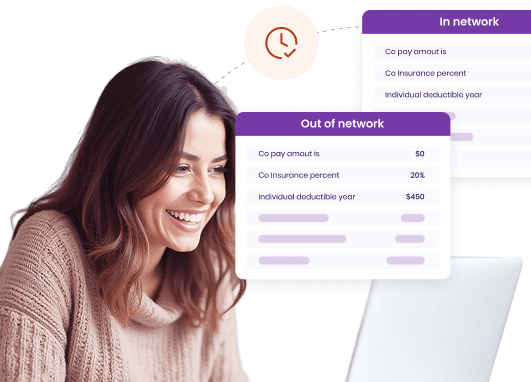
Simplify Exception Handling with AI and RCM Support
Resolve failed requests seamlessly through automated tagging, reference IDs, and direct routing to RCM teams for fast closure.
Stay Ahead with Proactive Alerts and Renewals
Stay ahead of expirations as SPRY identifies inactive plans and resubmits renewals automatically to keep patients cleared.
Don't Just Take Our Word For It.





-min%20(1).webp)
.webp)