Webinar: Beyond Fee for Service Direct-to-Employer Care for Clinics Built to Last | Featuring Scott Hebert
Register Now



.svg)
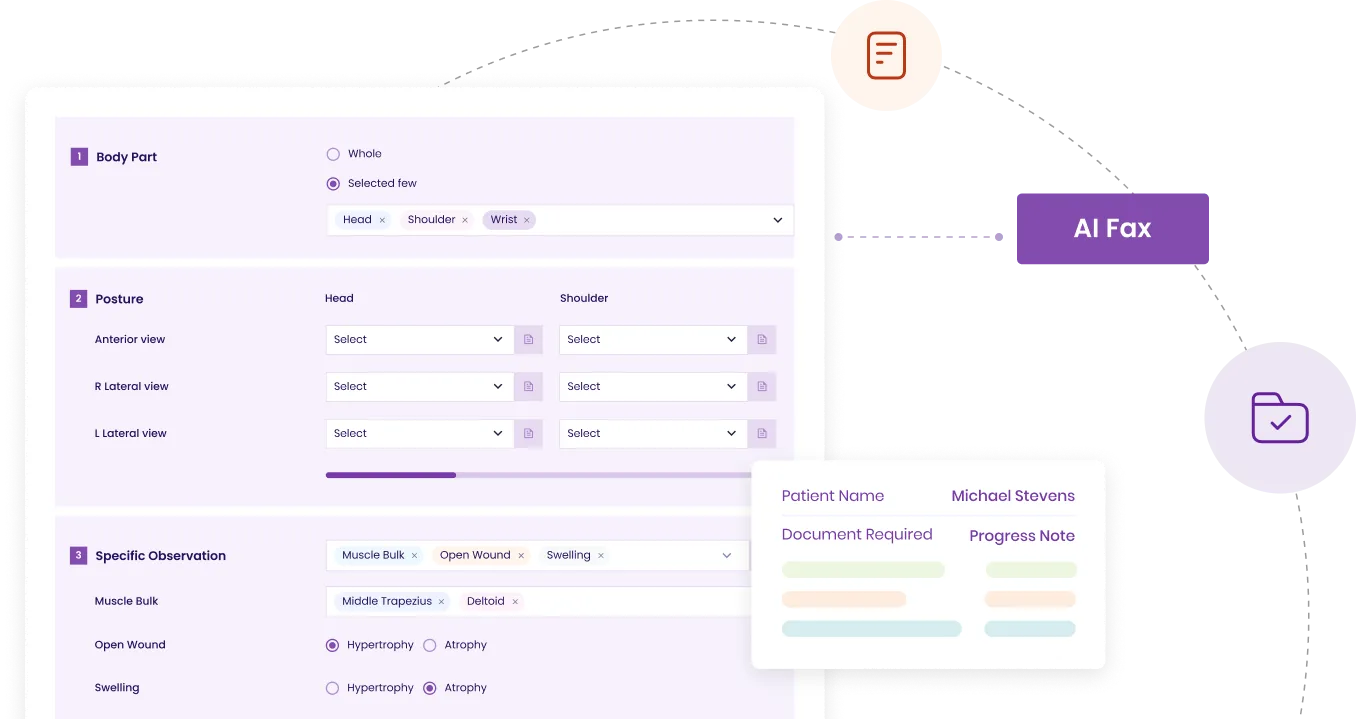
Patient data from Initial Evaluations automatically transfers to Follow-Ups and Progress Notes, reducing redundant entry.

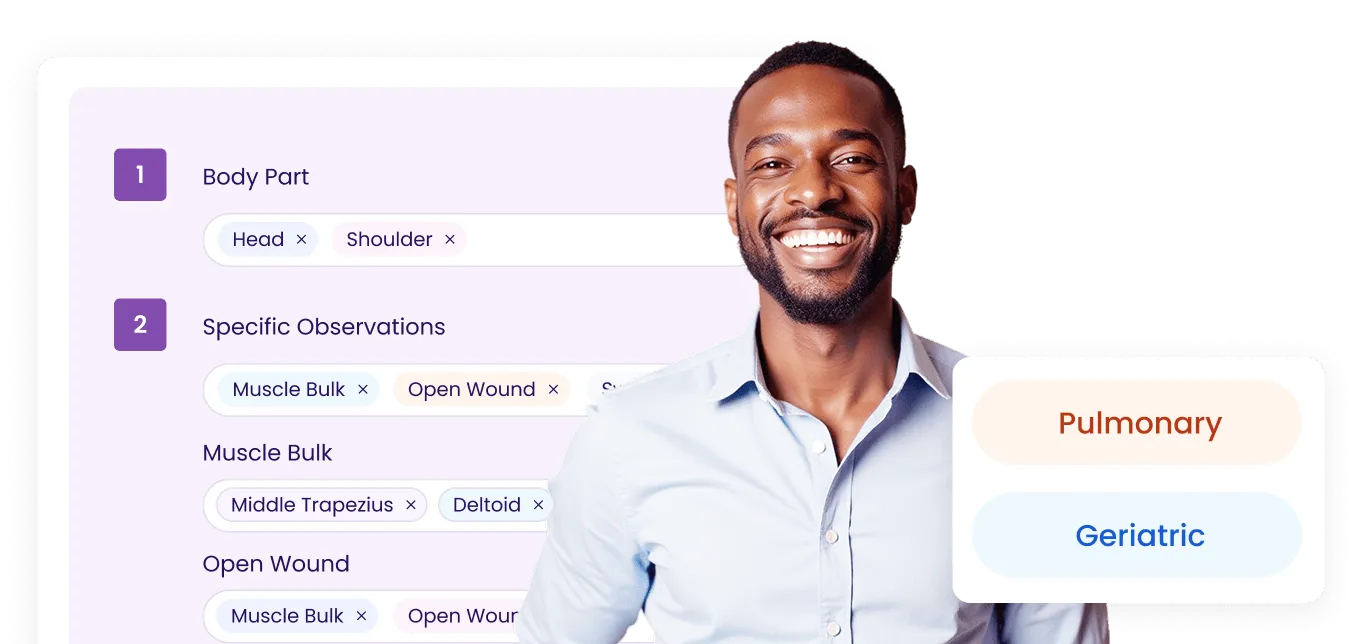
Supports various therapy disciplines within a single, unified system.
Real-time alerts for Medicare and
insurance-specific documentation requirements.
.webp)
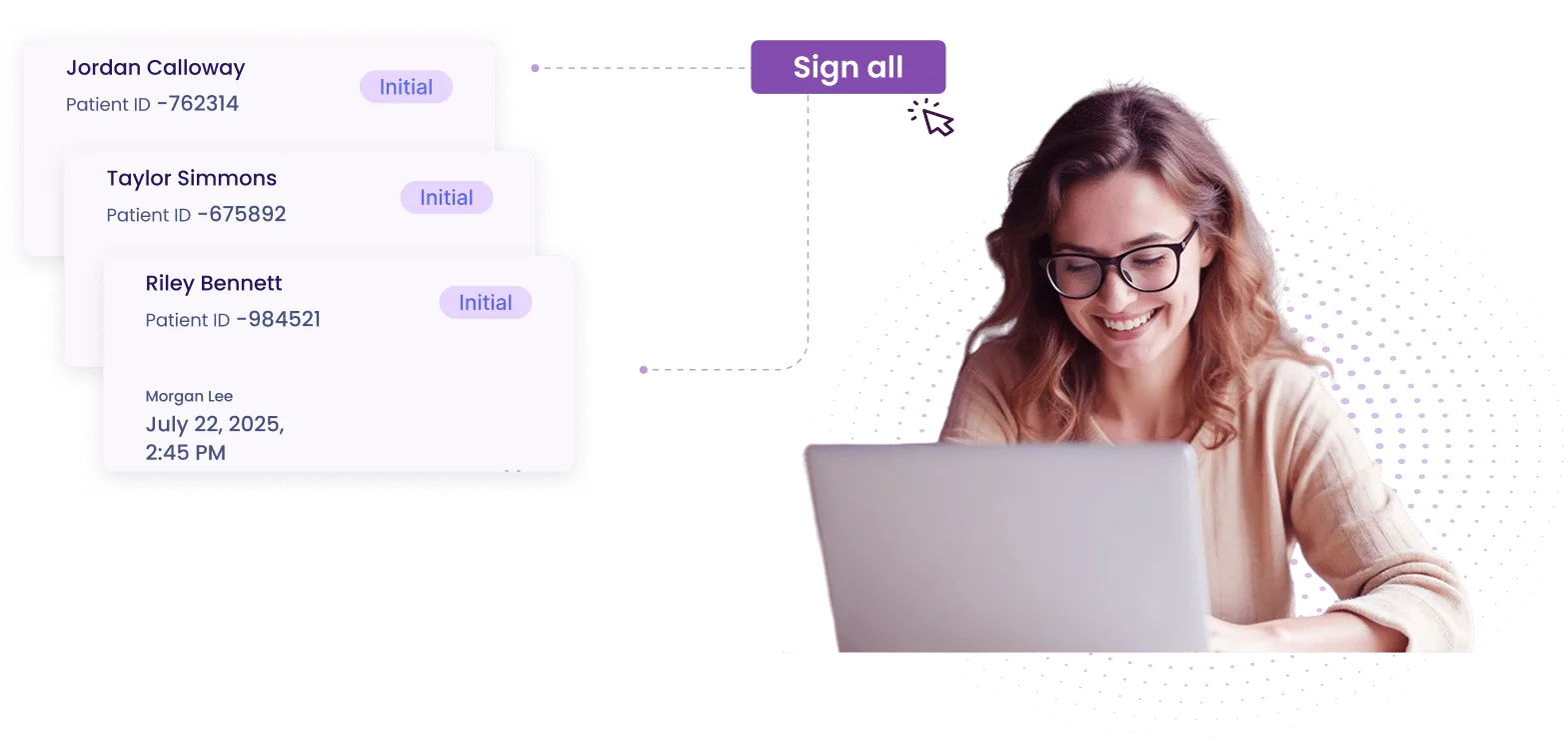
Therapists can easily review, approve, or request edits on notes, streamlining documentation oversight while maintaining full compliance.
Instantly send finalized notes to referring physicians for improved collaboration.
Tailored SOAP workflows that adapt to different therapy specialties.
.webp)
SPRY’s AI Scribe auto-generates SOAP notes from therapist-patient interactions in under 2 minutes, reducing documentation time by up to 70%. Paired with customizable templates and macros, therapists can complete accurate and audit-ready notes in minutes without manual typing.


Need more help? Reach out to us.
Real-time alerts flag Medicare and payer-specific issues.
Yes, notes can be securely faxed in seconds.
Yes, templates are fully customizable by discipline.
Yes, dropdowns for goals and objectives are available.
Yes, bulk co-signing is supported for efficiency.
Yes, therapist-defined goals can auto-fill across notes.
Info flows automatically from evals to progress notes.
It captures key visit details for quick review.