Podcast #5: From Taboo to Truth – The Real Story of Pelvic Floor Therapy with Hayley Kava
Watch Now
Try our Free Google Review Manager by SPRY for Rehab Therapy clinics
Try For Free




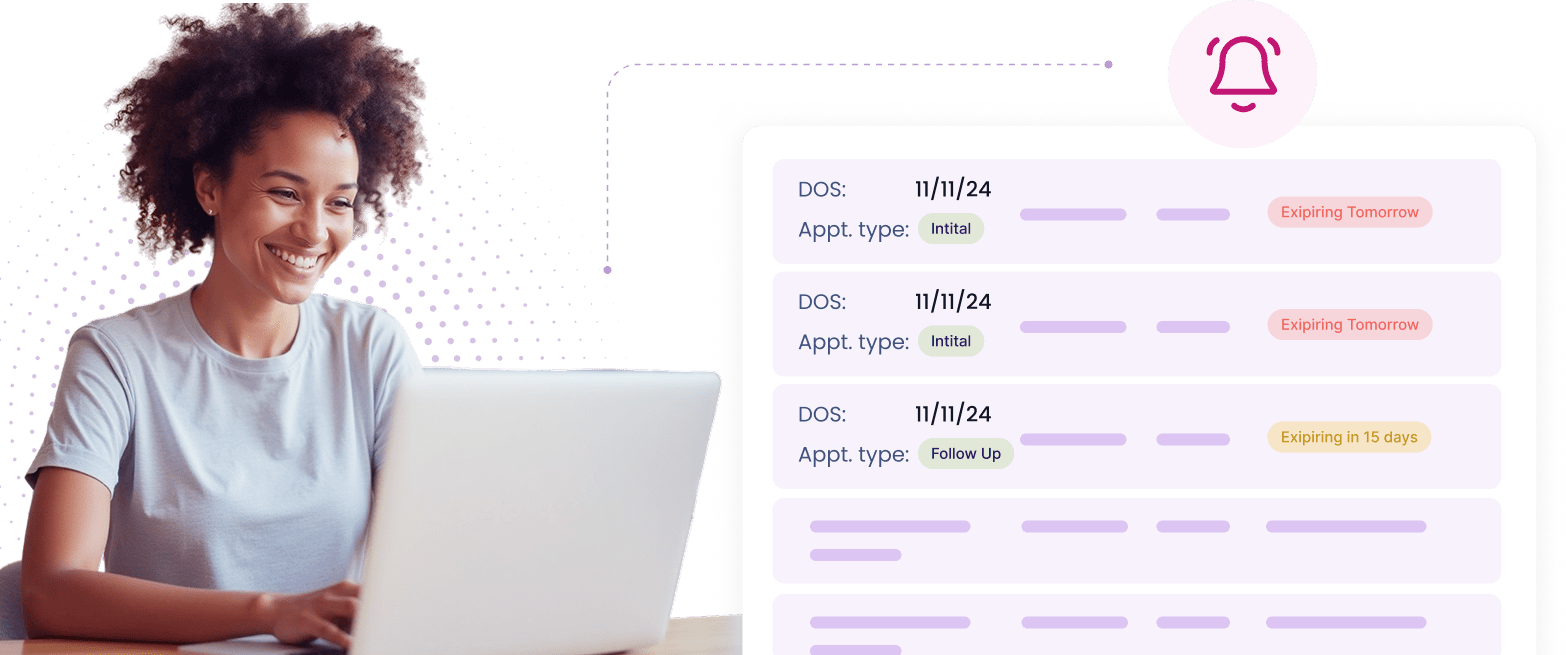
Automatically notifies staff of expiring authorizations 1 and 2 weeks in advance, ensuring timely renewals.
Define payer-specific requirements, eliminating guesswork and reducing claim denials.
.webp)
Tracks authorized visits and expiration dates, with adjustments that account for previously consumed visits.
.webp)
Authorization IDs automatically flow into CMS claim forms without manual intervention.
.webp)
Handles complex rules across different payers within a single system.

How It Works: Set Rules, Track Approvals, Automate Renewals






Need more help? Reach out to us.
SPRY Pre-Auth automates the prior authorization process for physical therapy clinics, reducing manual data entry, minimizing errors, and accelerating approvals.
SPRY supports a wide range of insurance pre-authorization needs, including those for Medicare, Medicaid, workers’ compensation, and commercial payers.
By automating form submission and eliminating manual bottlenecks, SPRY cuts down the turnaround time by up to 60%, enabling quicker patient care.
Absolutely. SPRY follows HIPAA-compliant practices to safeguard all patient and authorization data.
SPRY is designed to be intuitive and user-friendly. However, onboarding support and training are provided to ensure your team can maximize its efficiency.
SPRY uses AI to auto-fill forms, verify details, and submit pre-auth requests, saving you 6-10 minutes per submission and reducing the risk of errors.
Yes! SPRY’s AI-driven process reduces errors by up to 80%, ensuring accurate submissions and fewer rejections.
SPRY’s pre-auth system integrates seamlessly with its own EMR and billing platform, ensuring smooth workflows without double data entry.
Faster approvals mean patients start their treatment sooner, without unnecessary delays caused by manual authorization processes.
Yes! You can schedule a free demo to see how SPRY simplifies and accelerates the prior authorization process.