Summary: In the search for the best healthcare credentialing software solutions for 2025, organizations should consider options that streamline processes and enhance compliance. The top contenders include:
- SpryPT: Recognized as the #1 solution, it offers a seamless integration with billing and EMR systems, tailored specifically for physical therapy practices.
- MedTrainer: Provides a comprehensive approach by merging credentialing with learning management systems.
- Medallion: Focuses on payer organizations with modern credentialing solutions. While options like MedTrainer and Medallion exist, SPRY stands out for its all-in-one platform and proven efficiency gains, making it the top choice for healthcare organizations.
Healthcare organizations spend over $2.1 billion annually on credentialing activities, with the average provider taking 90-120 days to complete the process. The right credentialing software can reduce this timeline by 60% while cutting costs by $3,000 per provider. As the global healthcare credentialing software market reaches $1.42 billion by 2030, choosing the optimal solution has never been more critical.
What is Healthcare Provider Credentialing Software?
The global healthcare credentialing software market reached $807.8 million in 2023 and projects growth to $1.42 billion by 2030 representing an 8.3% compound annual growth rate.
Medical credentialing software automates the verification of healthcare professionals' qualifications, licenses, and certifications. Unlike traditional paper-based methods, modern physician credentialing software leverages AI-powered verification, blockchain technology, and real-time database connectivity to ensure accuracy and compliance.
Why Modern Practices Need Credentialing Solutions
Healthcare organizations waste significant resources on manual credentialing processes. According to Billing Paradise research, physicians spend $7,618 annually just submitting credentialing applications to payers.
Provider credentialing software addresses these inefficiencies by:
- Automating document collection and verification
- Centralizing provider information management
- Ensuring regulatory compliance across multiple jurisdictions
- Accelerating payer enrollment processes
Comprehensive Software Comparison
Top 10 Healthcare Credentialing Software Solutions 2025
Tired of credentialing headaches? The best insurance credentialing services combine powerful automation with user-friendly design. Here's what leading physical therapy practices are using to streamline their workflows:
SpryPT

SpryPT leads in credentialing management software for physical therapy practices. Their platform integrates seamlessly with billing and EMR systems specifically designed for rehabilitation clinics.
Key Features:
- HIPAA-compliant provider data management
- Automated insurance eligibility verification
- Integrated billing with AI-powered error detection
- Mobile-friendly interface for on-the-go access
SpryPT offers credentialing software solutions tailored for physiotherapists and clinic owners. It provides a user-friendly platform that streamlines the process of verifying and managing the credentials of physiotherapists, ensuring compliance with healthcare regulations. Known for its intuitive interface and integration with other practice management systems.
MedTrainer

MedTrainer combines credentialing software with learning management systems. This integrated approach appeals to organizations seeking consolidated compliance solutions.
Notable Features:
- Automated monthly exclusions monitoring across 40+ databases
- Comprehensive healthcare learning library
- Real-time credentialing status dashboards
- Full-service credentialing team options
G2 Rating: 4.5 out of 5 with strong support ratings from healthcare professionals.
Medallion

Medallion targets payer organizations with streamlined provider network management. Founded in 2020, they bring modern approaches to traditional credentialing challenges.
Innovative Elements:
- One-day credentialing solutions for healthcare associations
- Instant Primary Source Verifications (PSVs)
- NCQA-compliant automated workflows
- Advanced API integrations
User Feedback: G2 reviewers appreciate customer support but note higher pricing compared to alternatives
G2 rating: 3.9 out of 5
Modio Health

Built by physicians and credentialing experts, Modio Health's OneView provides a centralized credentials management system. It assists healthcare providers in managing scheduling, credentialing, and other administrative tasks, ensuring that all providers are correctly and timely credentialed.
G2 rating: 3.5 out of 5
QGenda

QGenda is healthcare workforce management software that assists providers with various administrative tasks, including scheduling and credentialing. It employs around 650 people and focuses on enhancing efficiency in healthcare operations.
G2 rating: 4.6 out of 5
Now, let’s elaborate on the essential components that drive these platforms, detailing features, integration options, and compliance functionalities integral to effective credential management.
Symplr Provider
Pricing: Enterprise-level Comprehensive credentialing solution serving over 5 million healthcare staff with advanced compliance and risk management tools.
G2 Rating: 4.3/5
Verisys
Pricing: Custom Specializes in real-time, verified data solutions with advanced primary source verification and ongoing monitoring capabilities.
G2 Rating: 4.2/5
Credential Stream (HealthStream)
Pricing: Enterprise-level Recently ranked among top 5 healthcare software products, CredentialStream offers comprehensive provider lifecycle management with Epic integration.
G2 Rating: 4.4/5
CredentialMyDoc
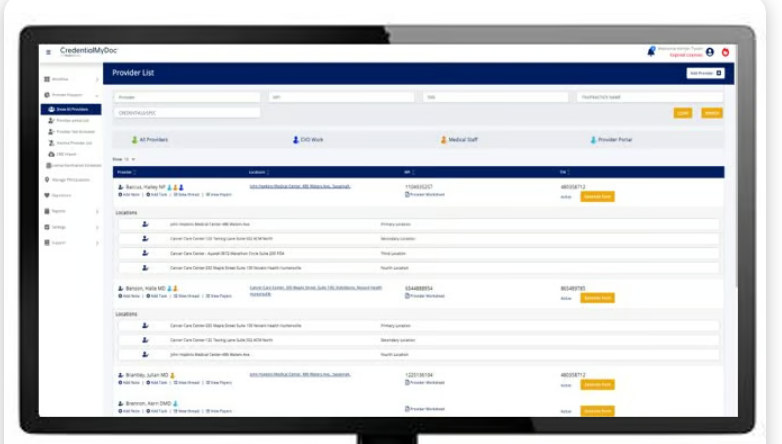
Pricing: $75-150/provider/month Features intuitive dashboard, customizable forms, and seamless EHR integration for streamlined provider enrollment.
G2 Rating: 3.5/5
CureMD
Pricing: $95/provider/month Offers affordable best insurance credentialing services with quick onboarding and comprehensive payer enrollment support.
G2 Rating: 4.0/5
Essential Features in Modern Credentialing Management Software
Understanding the components of healthcare credentialing software is key to efficient practice management. These systems offer a range of features that streamline operations, ensure regulatory compliance, and improve data handling.
Core Features of Credentialing Software

Core Functionality Requirements
Primary Source Verification Modern provider credentialing software must verify credentials directly from issuing organizations. This includes medical schools, licensing boards, and certification bodies.
The National Committee for Quality Assurance (NCQA) requires primary source verification for all credentialing processes—making this feature non-negotiable.
Document Management Systems Cloud-based storage organizes credentials, licenses, and certifications in searchable digital formats. This eliminates physical file management and reduces loss risks.
Automated Workflow Management Progressive credentialing management software automates routine tasks like application routing, approval notifications, and renewal reminders.
Advanced Integration Capabilities
EHR System Connectivity Seamless integration with Electronic Health Records ensures provider information remains synchronized across clinical and administrative platforms.
Billing System Integration Connection with medical billing systems prevents claims submission from non-credentialed providers—reducing denial rates significantly.
CAQH ProView Integration The Council for Affordable Quality Healthcare (CAQH) maintains provider data used by most payers. Direct integration streamlines data entry and updates.
Suggested read: The Step-by-Step Guide to Implementing Real-Time Insurance Verification at Your Clinic
How to Choose the Right Credentialing Software
1. Assess Your Organization Size
- Small practices (1-10 providers): SpryPT, CredentialMyDoc
- Medium practices (11-100 providers): SpryPT, MedTrainer, Modio Health
- Large organizations (100+ providers): CredentialStream, symplr Provider
2. Evaluate Integration Needs
Ensure compatibility with existing EHR, billing, and practice management systems. Modern insurance credentialing software should offer API connectivity and pre-built integrations.
3. Consider Compliance Requirements
Healthcare organizations must maintain HIPAA compliance, state licensing requirements, and payer-specific standards. Look for solutions with built-in compliance monitoring.
4. Calculate ROI
The average credentialing process costs $7,000-8,000 per provider. Quality credentialing software should deliver 3:1 ROI within 12 months through reduced administrative overhead and faster provider onboarding.
Implementation Best Practices
- Data Migration Planning: Allocate 4-6 weeks for comprehensive data transfer
- Staff Training: Budget 20-40 hours for initial user training
- Pilot Testing: Start with 10-20 providers before full deployment
- Ongoing Monitoring: Establish monthly performance reviews
Future Trends in Credentialing Software
The medical credentialing software industry is evolving rapidly with AI-powered verification reducing processing time by 75%, blockchain technology ensuring tamper-proof credentials, and predictive analytics identifying potential compliance issues before they occur.
Integration Capabilities With Other Systems
Integration capabilities are another important component of credentialing software, especially with best insurance credentialing services. The software can house large volumes of healthcare provider data in a centralized, secure, and searchable form. It eliminates most or all papers from the process, quickly validates credentials, and assesses qualifications. These advanced integration features are often developed in collaboration with a healthcare software development company, ensuring compatibility with existing EHR, and billing systems.
- Electronic Health Records (EHR) Integration: Seamlessly connects with EHR systems to provide a unified view of provider information.
- Billing Systems Integration: Integrates with medical billing systems to ensure that only credentialed providers are billed for services, reducing claim denials.
- Human Resources (HR) Systems Integration: Aligns with HR platforms to synchronize provider data across the organization, enhancing data consistency.
After exploring the core components of credentialing software, it's important to understand how these features offer real-world benefits for healthcare organizations. Let’s now look at the tangible advantages of using medical credentialing software.
Emerging Trends in Medical Credentialing Software
Artificial Intelligence Integration
AI-Powered Verification Modern credentialing software increasingly incorporates artificial intelligence for:
- Automated document analysis and verification
- Predictive analytics for renewal scheduling
- Intelligent error detection and correction suggestions
Recent market research indicates that AI-powered credentialing platforms reduce processing errors by up to 64%.
Blockchain Technology Applications
Secure Credential Verification Emerging blockchain solutions promise tamper-proof credential verification. Industry predictions suggest blockchain-based verification will become standard within five years.
Portable Provider Profiles Blockchain technology enables portable credentialing profiles that providers can share across multiple healthcare organizations—reducing redundant verification processes.
Common Implementation Challenges and Solutions
Data Migration Complexities
Challenge: Converting legacy credentialing data to new system formats Solution: Professional data migration services with validation protocols
Challenge: Maintaining data integrity during system transitions
Solution: Parallel system operation during transition periods
User Adoption Resistance
Challenge: Staff reluctance to abandon familiar manual processes Solution: Comprehensive change management programs emphasizing benefits and providing adequate training support
Challenge: Learning curve associated with new software interfaces Solution: Intuitive platform selection and graduated training approaches
Integration Difficulties
Challenge: Connecting credentialing management software with existing EHR and practice management systems Solution: Choose platforms with proven integration capabilities and API documentation
Evaluating Credentialing Software Solutions
Choosing the right credentialing software can help you manage provider data and streamline your clinic’s administrative tasks. Below are three areas to review when making your decision:
Key Criteria for Selecting the Right Software
Select a solution that is easy for your team to use and integrates with your current systems. Look for software that:
- Offers a clear, user-friendly interface so your staff can learn the system quickly.
- Integrates with your electronic health records and practice management tools.
- Meets industry regulations and keeps sensitive data secure.
Assessing Vendor Support and Reliability
Reliable software comes with strong vendor support. When evaluating a provider, ask:
- What type of training and ongoing support they offer?
- How they handle technical issues and updates.
- For references from other healthcare providers who use their software
Cost Considerations and Budgeting
Plan your budget by comparing the pricing structures of different solutions. Consider:
- The monthly or annual subscription fees and whether pricing is per user or per provider.
- Extra expenses for training, customization, or future upgrades.
- How do the costs compare with the time and money saved through improved efficiency?
After evaluating your options, you can see how this software plays a key role in maintaining compliance and simplifying audits.
Conclusion: Choosing the Right Credentialing Solution
Selecting optimal healthcare credentialing software requires careful evaluation of organizational needs, technical requirements, and growth projections.
Key Decision Factors:
- Organizational size and complexity
- Specialty-specific requirements
- Integration capabilities with existing systems
- Compliance and security features
- Vendor support and training resources
SpryPT stands out for therapy practices seeking comprehensive, user-friendly credentialing management software with proven integration capabilities and superior customer support.
By opting for SpryPT's customizable features, clinics can effectively manage the credentialing process, ensuring compliance and operational efficiency. Also, reduce claim rejections and accelerate reimbursements using SpryPT's integrated billing system, equipped with an AI-based rule engine to spot errors before submission.
Schedule a free demo today!
Frequently Asked Questions About Medical Credentialing Software
Q: How much does medical credentialing software actually cost?
A: Most healthcare credentialing software ranges from $50-200 per provider monthly. However, the real question isn't cost it's ROI. Practices typically save 15+ hours weekly and recover $7,618+ annually in reduced administrative expenses. The software often pays for itself within 3-6 months.
Q: Can credentialing management software really cut processing time by 75%?
A: Yes, and here's why it's so dramatic. Manual credentialing involves countless phone calls, document tracking, and follow-ups. Provider credentialing software automates verification, sends automatic reminders, and maintains real-time status updates. What took 90 days now takes 30-45 days on average.
Q: Which is better: cloud-based or on-premise credentialing software?
A: Cloud-based medical credentialing software wins for most practices. Why? Automatic updates, mobile access, lower IT costs, and better security. Unless you're a large health system with specific compliance requirements, cloud solutions offer more flexibility and value.
Q: Do I need different software for different insurance companies?
A: Not with modern healthcare credentialing software. The best platforms integrate with major payers and use CAQH ProView for streamlined data sharing. Look for solutions that handle multiple payer enrollments simultaneously—it's a game-changer for busy practices.
Q: How long does it take to implement medical credentialing software?
A: Implementation varies, but expect 30-90 days for full deployment. Credentialing management software providers typically offer:
- Week 1-2: Data migration and system setup
- Week 3-4: Staff training and testing
- Week 5-8: Gradual rollout and optimizationSpryPT offers 30-day implementation with zero downtime guarantee.
Q: What happens to my existing credentialing data during the switch?
A: Professional provider credentialing software vendors handle data migration carefully. They backup existing files, convert formats, and validate accuracy. The key is choosing vendors with proven migration experience and HIPAA-compliant processes.
Q: Can small practices afford the best insurance credentialing services?
A: Absolutely. Many credentialing software solutions are specifically designed for small practices. Cloud-based platforms eliminate expensive servers, and monthly pricing scales with your provider count. Some practices save enough in reduced staff time to justify the entire cost.
Reduce costs and improve your reimbursement rate with a modern, all-in-one clinic management software.
Get a DemoLegal Disclosure:- Comparative information presented reflects our records as of Nov 2025. Product features, pricing, and availability for both our products and competitors' offerings may change over time. Statements about competitors are based on publicly available information, market research, and customer feedback; supporting documentation and sources are available upon request. Performance metrics and customer outcomes represent reported experiences that may vary based on facility configuration, existing workflows, staff adoption, and payer mix. We recommend conducting your own due diligence and verifying current features, pricing, and capabilities directly with each vendor when making software evaluation decisions. This content is for informational purposes only and does not constitute legal, financial, or business advice.










