BEST Physical Therapy improves clean claim rates to 95% with SPRY
Let's Talk.png)

Clinic: BEST Physical Therapy (now BEST Health, Wellness, Performance), a multi‑location practice with over 50 therapists.
Challenge: Fragmented workflows from separate EMR and billing systems led to coding errors, underpayments and unresolved denials.
Transition: SPRY combined EMR and billing into one platform, adding automated coding, authorization management, real‑time payment tracking and structured denial management.
Impact: Clean‑claim rates climbed to 95%, claim processing time dropped by 30 % and cash flow improved.
Client Overview
Founded by Marc Douek, BEST Physical Therapy (now rebranded as BEST Health, Wellness, Performance) is a multi-location group with more than 50 therapists.
The clinic is dedicated to delivering high-quality care across multiple disciplines, but fragmented claim workflows were threatening profitability and staff efficiency.
The Challenge
BEST Physical Therapy struggled with a disjointed system, switching between Jane (EMR) and Office Ally (billing).
These limitations caused ripple effects across the business:
Coding Errors — from manual entry of CPT and ICD-10 codes, leading to frequent denials.
Incomplete Documentation — that stalled approvals and disrupted billing accuracy.
Underpayment by Insurers — due to limited visibility into claim statuses.
Neglected Denial Appeals — many denied claims were left unresolved.

Why They Chose SPRY
The clinic needed a single, integrated system that could remove manual steps, prevent revenue leakage, and improve visibility into financial performance.
SPRY stood out for:
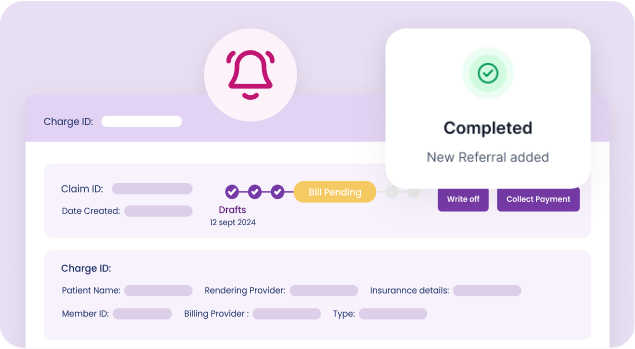
Automated Coding Templates to eliminate manual CPT/ICD-10 entry
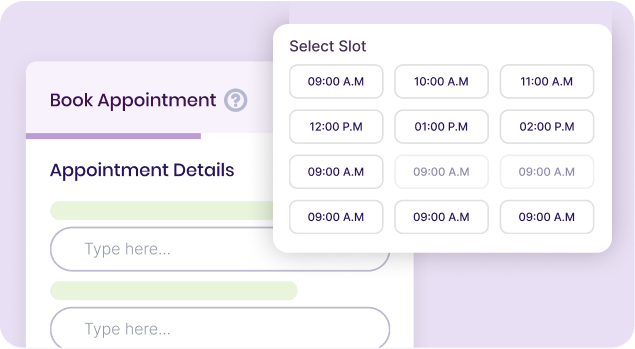
Authorization Management that flagged missing details before claim submission
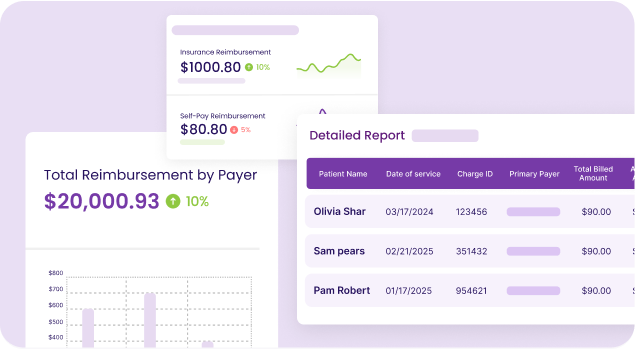
Real-Time Payment Tracking with a financial dashboard to spot underpayments
Structured Denial Management that automated appeals and prevented revenue loss
Solutions in Action
SPRY replaced the fragmented Jane + Office Ally setup with one platform designed to handle the entire workflow:
EMR + Billing Integration, no more manual data transfers
Automated Coding populated directly from treatment notes
Authorization Alerts to prevent delays before claim submission
Payment Tracking with real-time visibility and underpayment alerts
Denial Management Tools that ensured appeals were processed
Outcomes with SPRY
SPRY automated manual processes and freed staff for higher-value work.
SPRY allowed the clinic to redirect staff time and resources to patients.
SPRY strengthened BEST’s financial performance and cash flow.
The SPRY Advantage
With SPRY, BEST Physical Therapy achieved:
Eliminated manual entry errors: unifying EMR and billing removes duplicate data entry and reduces mistakes.
Streamlined operations: automation frees staff to focus on patient care instead of billing tasks.
Improved cash flow: higher clean‑claim rates and faster approvals mean payments arrive sooner.
Complete revenue visibility: real‑time dashboards highlight underpayments and optimise recovery.
Ongoing tailored support: a dedicated team continuously refines processes and ensures success.
