Black Book Research ranks SPRY #1 for PT/OT Rehab in Ambulatory EHR Excellence 2026
Learn More


Trusted by leading rehab therapy clinics
















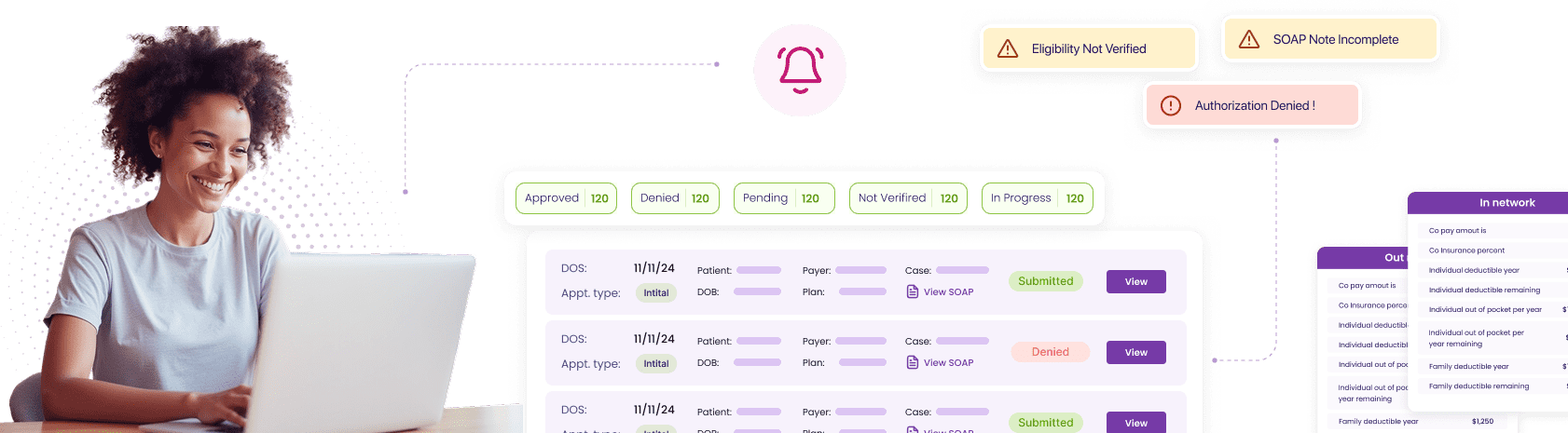
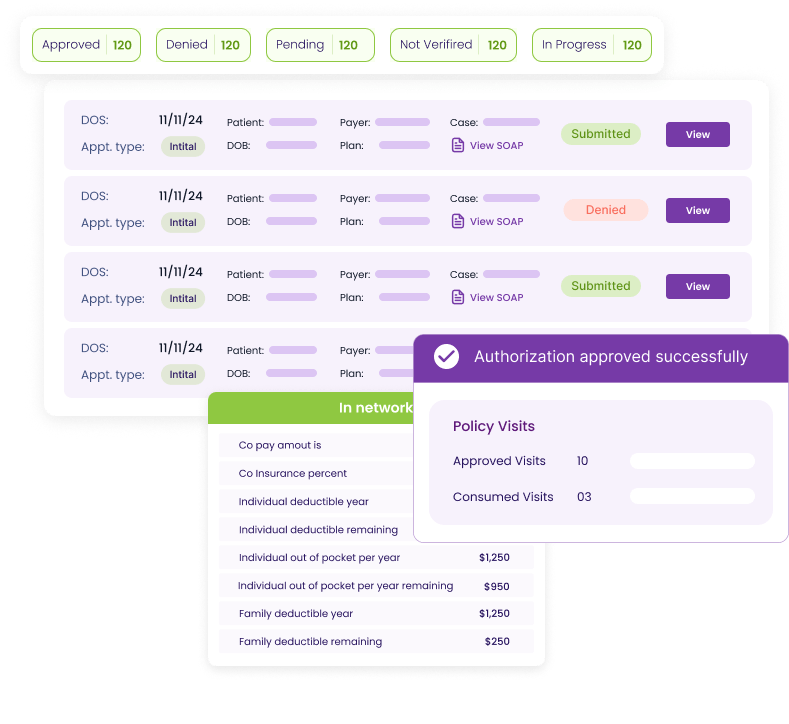
Streamline insurance operations by unifying eligibility, coverage, and authorizations in one system—eliminating portal-hopping and manual entry.
Automate submissions with AI that files requests, attaches documentation, and flags issues early.

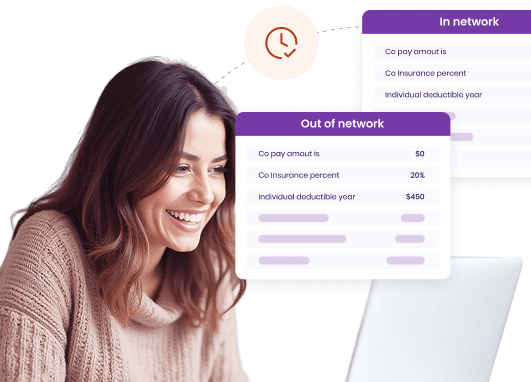
Confirm coverage instantly with copays, deductibles, and limits verified at scheduling.
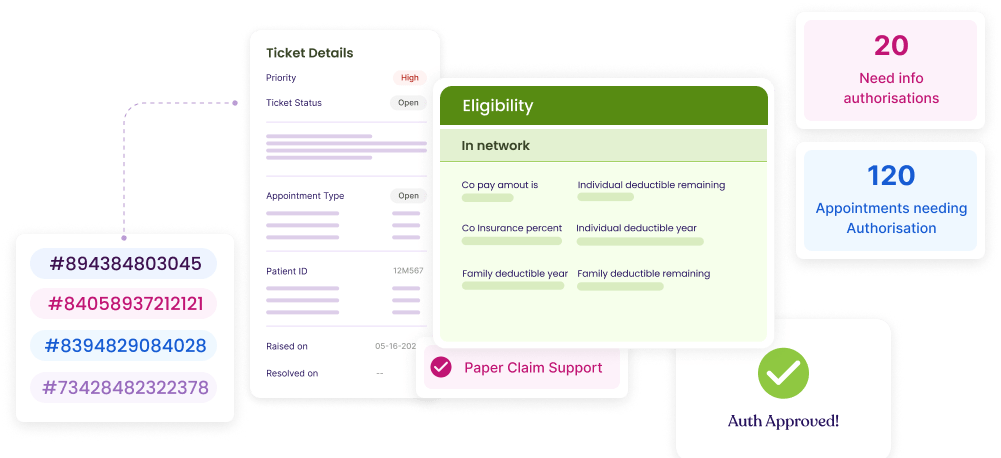
Resolve failed requests seamlessly through automated tagging, reference IDs, and direct routing to RCM teams for fast closure.
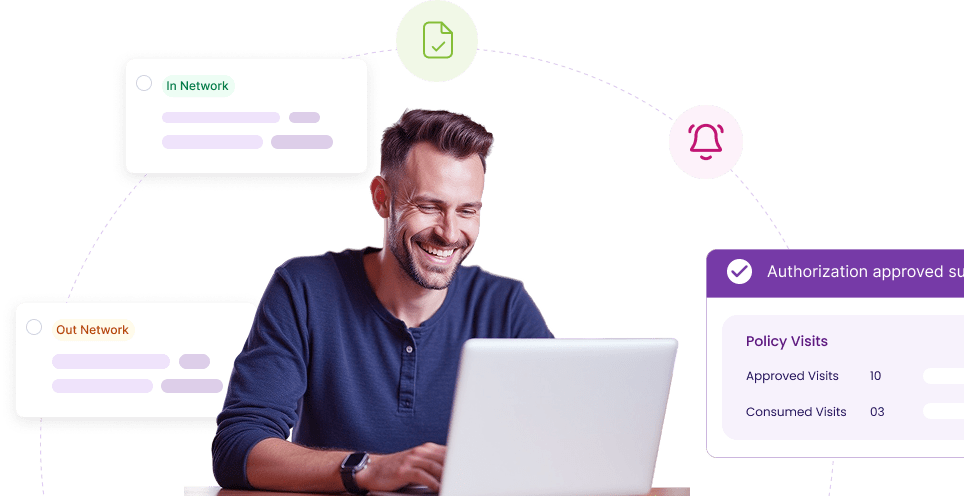
Stay ahead of expirations as SPRY identifies inactive plans and resubmits renewals automatically to keep patients cleared.






















Need more help? Reach out to us.
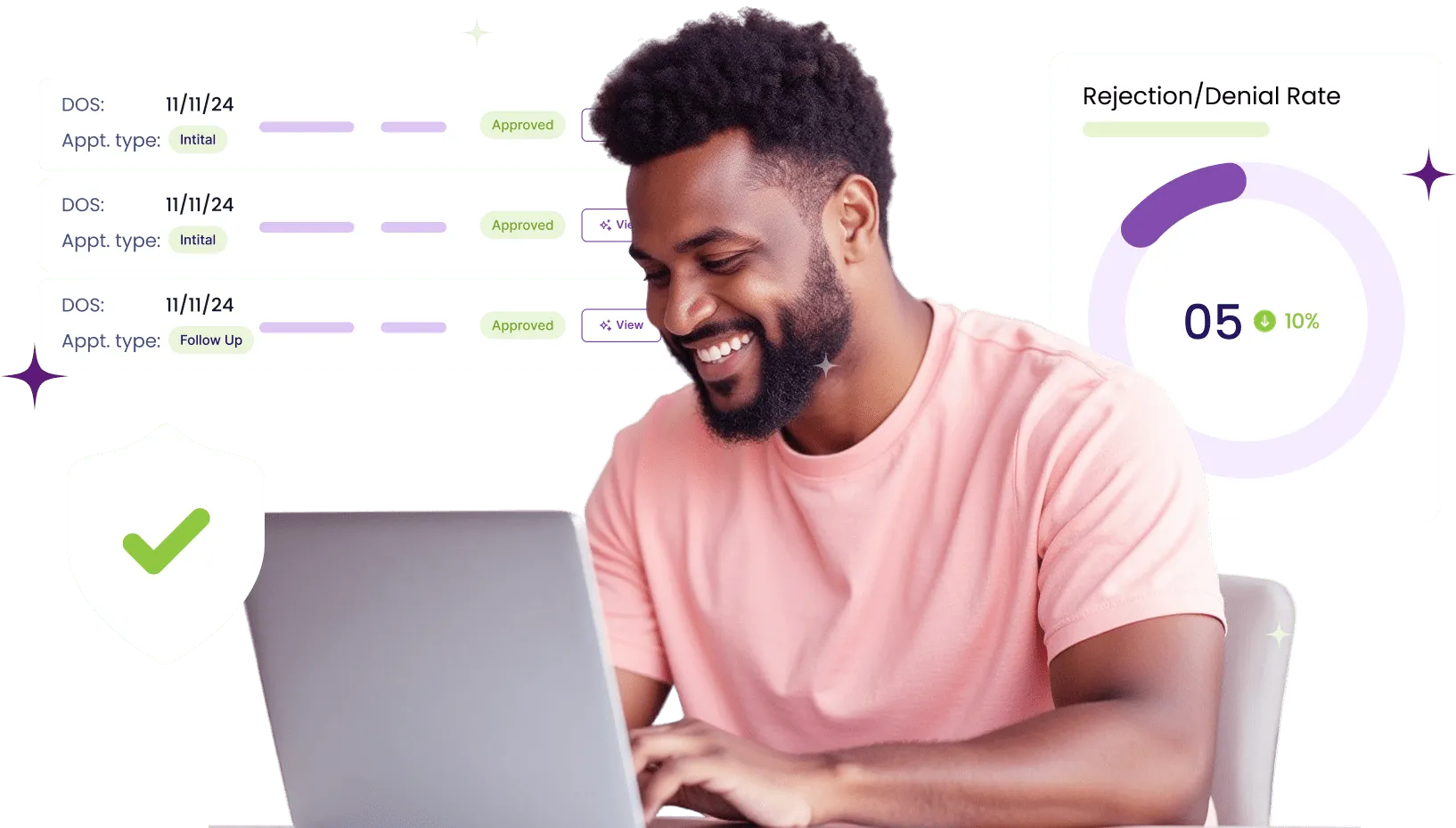
SPRY automates up to 80% of authorization requests across major payers such as Carelon/BCBS, UnitedHealthcare, and Humana. Our AI agents pull clinical notes and CPT codes directly from therapist documentation, complete payer-specific forms, and submit them through portals or APIs. Staff only step in when exceptions are flagged, meaning your team spends far less time on repetitive tasks and far more time on patient care.
Yes. SPRY already supports leading payer portals and is continuously expanding coverage. Our AI agents adapt to website changes automatically, support two-factor authentication (via SMS/email codes or Google Authenticator), and securely vault credentials for re-submissions. Every transaction is logged with a full audit trail, giving clinics confidence in compliance and visibility across all requests.
Failed or complex cases are tagged with unique reference IDs, logged in the dashboard, and routed to your RCM team for follow-up. Context from the payer is preserved, so staff can resolve issues quickly without starting from scratch. This ensures 100% of requests are tracked to completion, preventing lost revenue and missed care.
SPRY’s system re-verifies all scheduled patients’ coverage every night. If a payer makes mid-month changes — such as policy lapses, deductible resets, or visit limit adjustments — the dashboard alerts staff before the patient arrives. This proactive check helps ensure cleaner first-pass claims, reduces same-day denials, and prevents awkward surprises at check-in.
The CMS Interoperability and Prior Authorization Final Rule requires certain electronic prior authorization processes by 2026. SPRY is fully aligned with these requirements through FHIR-compatible APIs, automated audit trails, and payer-compliant submissions. By adopting SPRY now, clinics eliminate the need for costly system upgrades later — and stay ahead of regulatory deadlines.
Most clinics are live in under three business days. Setup involves configuring payer lists, enrolling NPI credentials, and syncing schedules. From day one, clinics see eligibility results in seconds, authorizations submitted automatically, and proactive alerts for expirations or inactive plans. SPRY is EMR-agnostic, so you can start with the dashboard and later integrate with your EMR for an even more seamless workflow.