Summary: Choosing the right EMR system in 2025 is crucial for healthcare professionals facing increasing administrative burdens and the need for efficient workflows. This guide compares the top EMR systems, highlighting their strengths and weaknesses. While options like Epic Systems and Cerner are notable, SPRY stands out as the #1 solution for its all-in-one platform, proven efficiency gains, and seamless integration capabilities, making it the best choice for enhancing patient care and reducing documentation overload.
Healthcare professionals face an overwhelming choice when selecting Electronic Medical Record (EMR) systems in 2025. With over 500 EMR solutions available, making the right decision requires understanding real-world performance, workflow integration, and long-term value.
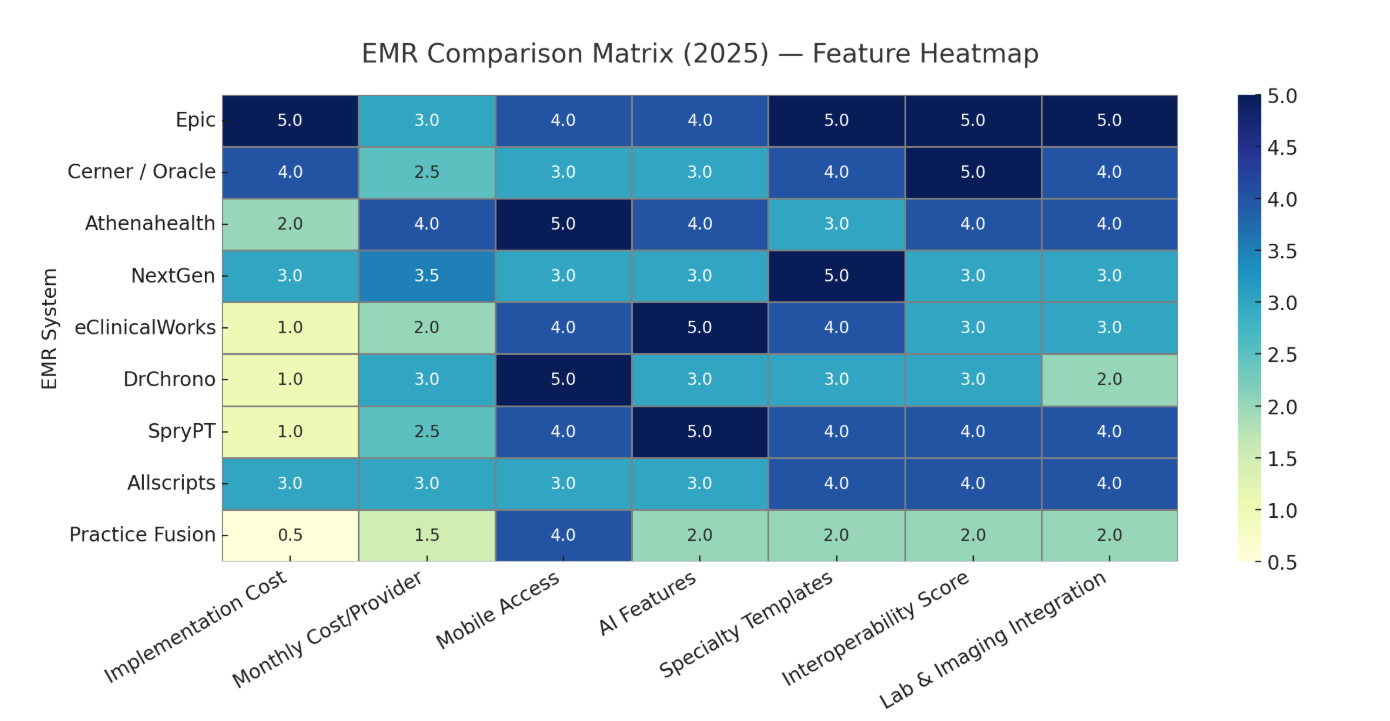
This comprehensive EMR comparison matrix analyzes the top EMR 2025 systems based on actual user experiences, clinical workflow efficiency, and measurable outcomes reported by healthcare practices across the United States.
Why EMR Selection Matters More Than Ever in 2025
According to the CDC's National Electronic Health Records Survey, 88.2% of office-based physicians now use EMR systems, with 77.8% relying on certified software. However, studies show that physicians spend an average of 15.5 hours weekly on administrative tasks, with much of this time attributed to inefficient EMR workflows.
The stakes are higher in 2025. Healthcare professionals need systems that reduce documentation burden, improve patient care coordination, and adapt to evolving telehealth requirements. Tools like an EMR comparison matrix can help providers evaluate platforms on critical factors such as mobile access for physicians, fastest implementation times, and lab imaging integration capabilities.
Key Challenges Healthcare Professionals Face
Research from the Healthcare Information Management Systems Society (HIMSS) identifies critical pain points:
- Documentation Overload: Physicians spend 4-6 hours daily interacting with EMR systems
- Workflow Disruption: Poor system integration creates additional administrative burden
- Usability Issues: 50% of EMR users report significant usability problems
- Interoperability Gaps: Limited data sharing between different healthcare systems
What is EMR Solutions Lab Imaging Integration (2025)?
Lab and imaging integration in EMR systems allows automated data flow from diagnostic systems like:
- Laboratory Information Systems (LIS)
- Picture Archiving and Communication Systems (PACS)
- Radiology Information Systems (RIS)
In 2025, this integration is more critical than ever because:
- CMS is pushing for interoperability and data exchange standards (FHIR)
- AI-powered imaging diagnostics are growing fast
- Value-based care models require faster test-to-treatment workflows
Top EMR 2025 System: Performance-Based Rankings
Epic Systems: The Enterprise Leader
Best For: Large health systems, hospitals, academic medical centers
Epic dominates the enterprise market with comprehensive functionality and strong interoperability. However, implementation complexity and cost make it challenging for smaller practices.
Key Strengths:
- Robust population health management tools
- Excellent interoperability with 95% of hospitals
- Advanced analytics and reporting capabilities
- Strong patient portal functionality
Limitations:
- Implementation costs ranging from $500,000 to $2 million
- Extensive training requirements (4-8 weeks)
- Complex interface that can slow clinical workflows
User Satisfaction: 73% (KLAS Research 2024)
Cerner (Oracle Health): Government and Academic Focus
Best For: Government facilities, academic institutions, large hospital networks
Cerner's acquisition by Oracle brings enhanced cloud capabilities but maintains focus on enterprise-level healthcare organizations.
Key Strengths:
- Strong security protocols for government compliance
- Robust population health analytics
- Integration with Oracle's business intelligence tools
- Comprehensive revenue cycle management
Limitations:
- Inconsistent user interface across modules
- Performance issues during peak usage
- Limited customization for specialty practices
User Satisfaction: 68% (KLAS Research 2024)
Athenahealth: Cloud-Native Innovation
Best For: Ambulatory practices, specialty clinics, growing healthcare organizations
Athenahealth pioneered cloud-based EMR delivery and continues to innovate with AI-powered features and workflow optimization.
Key Strengths:
- Native cloud architecture with 99.9% uptime
- Integrated revenue cycle management
- Strong mobile access capabilities
- Automated clinical documentation features
Limitations:
- Higher per-provider costs than competitors
- Limited hospital integration capabilities
- Frequent updates can disrupt established workflows
User Satisfaction: 82% (KLAS Research 2024)
NextGen Healthcare: Specialty Practice Excellence
Best For: Specialty practices, behavioral health, cardiology, orthopedics
NextGen excels in providing specialty-specific templates and workflows, making it popular among specialized medical practices.
Key Strengths:
- Extensive specialty-specific templates
- Advanced clinical decision support
- Strong patient engagement tools
- Flexible customization options
Limitations:
- Higher costs for smaller practices
- Occasional system performance issues
- Complex reporting features
User Satisfaction: 75% (KLAS Research 2024)
eClinicalWorks: AI-Powered Documentation
Best For: Primary care practices, multi-specialty groups, telehealth-focused practices
eClinicalWorks leads in AI-powered documentation and patient engagement tools, making it attractive for practices prioritizing automation.
Key Strengths:
- Advanced AI documentation capabilities
- Comprehensive telehealth integration
- Strong patient portal features
- Competitive pricing structure
Limitations:
- Customer support inconsistencies
- Interface design feels outdated
- Occasional system downtime during updates
User Satisfaction: 71% (KLAS Research 2024)
EMR Solutions Mobile Access for Physicians 2025
Mobile accessibility has become critical as healthcare delivery evolves. The COVID-19 pandemic accelerated telemedicine adoption, making emr solutions mobile access for physicians 2025 a top priority.
Leading Mobile EMR 2025 Solutions
DrChrono: iPad-first design with comprehensive mobile functionality
- Native iPad application with full feature parity
- Real-time patient data synchronization
- Mobile-optimized charting interface
- Integrated telehealth capabilities
Athenahealth: Cloud-native mobile optimization
- Responsive web design across all devices
- Mobile patient portal integration
- Real-time appointment scheduling
- Secure messaging capabilities
Epic MyChart: Patient engagement leader
- Comprehensive patient portal access
- Provider mobile applications
- Real-time care team communication
- Mobile-optimized clinical workflows
EMR Summarization Solutions Compared
AI-powered EMR summarization solutions compared represent the future of clinical documentation. These tools use natural language processing to reduce documentation time and improve accuracy.
Leading AI Documentation Solutions
Nuance Dragon Medical One: Industry-standard voice recognition
- 99% accuracy rate for medical terminology
- Integration with major EMR systems
- Real-time transcription capabilities
- Specialty-specific vocabularies
Sprypt AI Clinical Assistant: Next-generation documentation automation
- Real-time ambient listening and transcription
- Intelligent note structuring and formatting
- Automated coding suggestions
- Contextual clinical decision support
Microsoft Healthcare Bot: Conversational AI integration
- Natural language understanding
- Integration with Epic and Cerner
- Automated patient intake processes
- Multi-language support capabilities
Abridge: AI-powered clinical conversations
- Real-time conversation analysis
- Automated clinical note generation
- Integration with major EMR platforms
- HIPAA-compliant processing
AI Documentation Impact Metrics
Studies show AI-powered documentation tools can:
- Reduce documentation time by 40-60%
- Improve clinical note accuracy by 35%
- Increase physician satisfaction scores by 25%
- Decrease administrative burden by 45%
Specialty-Specific EMR Solutions
Different medical specialties require tailored functionality. The emr feature comparison chart varies significantly based on specialty requirements.
Physical Therapy EMR Solutions
SPRY PT: Emerging PT-focused solution
- Modern user interface design
- Automated billing processes
- Treatment plan optimization
- Mobile-first architecture
WebPT: Industry-leading PT software
- Outcome measurement integration
- Exercise prescription tools
- Insurance authorization tracking
- Patient engagement portal
Mental Health EMR Leaders
TherapyNotes: Behavioral health specialist
- Comprehensive treatment planning tools
- Insurance verification automation
- Telehealth integration with session notes
- Outcome measurement tracking
TheraNest: Multi-disciplinary mental health
- Group therapy management
- Family therapy documentation
- Progress note templates
- Billing optimization features
Implementation Success Factors
Successful EMR implementation requires strategic planning and change management. Research shows that 60% of EMR implementations face significant challenges.
Critical Success Factors
Leadership Commitment: Executive sponsorship and physician champions
Workflow Analysis: Detailed current-state and future-state mapping
Training Programs: Comprehensive user education and support
Data Migration: Accurate historical data transfer processes
Go-Live Support: 24/7 technical support during transition
Implementation Timeline Benchmarks
- Small Practices (1-5 providers): 3-6 months
- Medium Practices (6-25 providers): 6-12 months
- Large Organizations (25+ providers): 12-24 months
- Health Systems (Multiple locations): 18-36 months
Cost Analysis and ROI Considerations
EMR investment requires careful financial analysis. Total cost of ownership includes implementation, training, ongoing support, and system upgrades.
Cost Categories
Implementation Costs:
- Software licensing fees
- Hardware requirements
- Data migration expenses
- Training and support costs
Ongoing Costs:
- Monthly subscription fees
- Technical support contracts
- System upgrade expenses
- Additional user licenses
ROI Calculation Framework
Healthcare practices typically see EMR ROI through:
- Reduced administrative costs (25-40% reduction)
- Improved billing accuracy (15-25% increase)
- Enhanced patient throughput (10-20% improvement)
- Decreased transcription costs (80-100% elimination)
EMR Future Trends in EMR Technology
EMR 2025 will be shaped by emerging technologies and evolving healthcare delivery models.
Key Technology Trends
Artificial Intelligence Integration:
- Predictive analytics for patient care
- Automated clinical decision support
- Real-time risk assessment tools
- Personalized treatment recommendations
Interoperability Advancement:
- FHIR-based data exchange
- Real-time health information networks
- Cross-platform data sharing
- Patient-controlled health records
Patient Engagement Evolution:
- Wearable device integration
- Social determinants tracking
- Behavioral health monitoring
- Personalized care plan delivery
Conclusion: Making the Right EMR Choice
Selecting the optimal EMR system requires balancing functionality, cost, and workflow integration. Healthcare professionals should prioritize systems that demonstrate measurable improvements in clinical efficiency and patient care outcomes.
The emr comparison matrix shows significant variation in capabilities, costs, and user satisfaction. Success depends on aligning system capabilities with specific practice requirements and ensuring comprehensive implementation support.
Consider engaging with EMR vendors for demonstrations, speaking with current users in similar practices, and conducting pilot implementations before making final decisions.
Sources and References:
- CDC National Electronic Health Records Survey, 2024
- HIMSS Electronic Health Record Association, 2024
- KLAS Research EMR User Satisfaction Report, 2024
- Medscape Physician Compensation Report, 2023
- American Medical Association Digital Health Study, 2024
- Healthcare Information Management Systems Society, 2024
Reduce costs and improve your reimbursement rate with a modern, all-in-one clinic management software.
Get a DemoLegal Disclosure:- Comparative information presented reflects our records as of Nov 2025. Product features, pricing, and availability for both our products and competitors' offerings may change over time. Statements about competitors are based on publicly available information, market research, and customer feedback; supporting documentation and sources are available upon request. Performance metrics and customer outcomes represent reported experiences that may vary based on facility configuration, existing workflows, staff adoption, and payer mix. We recommend conducting your own due diligence and verifying current features, pricing, and capabilities directly with each vendor when making software evaluation decisions. This content is for informational purposes only and does not constitute legal, financial, or business advice.










